Medical pharmacology
What is medical pharmacology ?
Medical pharmacology is the study of drugs and their interactions with the body. It involves the research, development, and evaluation of drugs used to prevent, diagnose, and treat various diseases and conditions. Medical pharmacologists use their knowledge of the mechanisms of action, side effects, and interactions of drugs to ensure their safe and effective use. They also study how drugs are absorbed, distributed, metabolized, and excreted in the body, as well as how genetics, age, and other factors can affect the way drugs work. Medical pharmacology plays a critical role in the development of new treatments for a variety of medical conditions and is essential for improving patient care.
Important Definations
1. Drug:
2. Medicine:
Drug characteristics
- Solid (Aspirin, Atropine).
- Liquid (Nicotine).
- Gaseous (Nitrous oxide).
3. Lipid solubility: Lipid solubility refers to the ability of a drug to dissolve in fat, which can affect how quickly it is absorbed and distributed in the body.
pKa: pKa is a measure of the acidity of a drug, which can affect its solubility and ionization state in the body.
4. Molecular weight: The molecular weight of a drug is a measure of its size and can affect its ability to cross cell membranes and bind to proteins.
- Most drugs have molecular weights between 100 and 1000.
- Some smaller (lithium) some larger (alteplase)
- Play an important role in specificity of action.
- Drug specificity is a way by which drug targets specific site.
- The smaller drug passes easily through body barriers and reached more sites than the larger one.
6. Route of administration: The route of administration refers to how the drug is taken into the body and can include oral, intravenous, topical, and other methods.
7. Bioavailability: Bioavailability is a measure of how much of a drug is absorbed into the bloodstream and reaches its site of action.
8. Metabolism: The metabolism of a drug refers to the processes by which the body breaks down and eliminates the drug, and can affect its efficacy and side effects.
- Code No.: e.g. TRO19622.
- Chemical: e.g. N-acetyl-p-aminophenol.
- Generic Name: acetaminophen or paracetamol.
- Trade Name: panadol, …etc.
Sources of Drugs
- Synthetic chemicals: Many drugs are synthesized in the laboratory using chemical reactions. This allows for the creation of specific compounds with well-defined structures and properties. e.g. (Aspirin).
- Natural products: Drugs can also be derived from natural sources, such as plants, animals, and microorganisms. These drugs can be isolated from the natural source or chemically modified to improve their therapeutic properties. eg. (Digoxin- Heparin-Lithium).
- Microorganisms: Some drugs are produced by microorganisms, such as bacteria and fungi. For example, antibiotics like penicillin and streptomycin are produced by bacteria.
- Recombinant DNA technology: This method involves the manipulation of DNA to produce specific proteins that can be used as drugs. For example, human insulin is produced using recombinant DNA technology. eg. (Insulin).
Drug-Body Interactions
- The actions of the drug on the body are termed pharmacodynamic processes.
- The actions of the body on the drug are called pharmacokinetic processes.
Drug –Drug Interaction
- Additive effects: This occurs when two drugs with similar mechanisms of action are taken together, leading to an increase in their combined effect, (1+2=3).
- Antagonistic effects: This occurs when two drugs with opposing mechanisms of action are taken together, leading to a reduction in their combined effect (1-1=0).
- Synergistic effects: This occurs when two drugs with complementary mechanisms of action are taken together, leading to an increased therapeutic effect compared to when each drug is taken alone(1+2=5) Ampiclox “ampicillin+cloxacillin”.
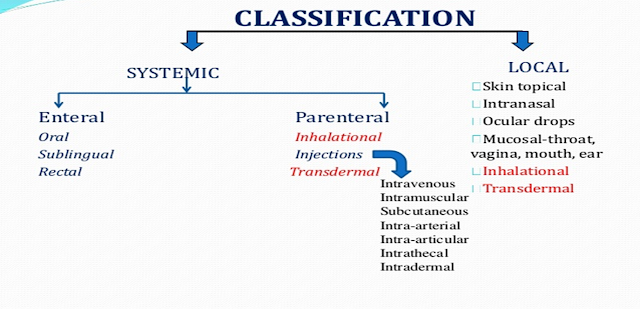
Routes of drug Administration
- Oral: This is the most common route of administration and involves taking a drug by mouth in the form of a pill, tablet, or liquid.
- Inhalation: This involves breathing in a drug in the form of a gas or mist, such as with an inhaler for the treatment of asthma.
- Topical: This involves applying a drug to the skin or mucous membranes, such as with a cream or ointment for the treatment of skin conditions.
- Parenteral: This involves administering a drug through injection, either intravenously (into a vein), intramuscularly (into a muscle), or subcutaneously (under the skin).
- Rectal: This involves administering a drug through the rectum in the form of a suppository.
- Intranasal: This involves administering a drug through the nasal passages, such as with a nasal spray.
 | |
| Routes of drug Administration |
The choice of route of administration depends on several factors, including the type of drug, its intended effect, the patient's age and overall health, and the presence of any contraindications to a particular route of administration. The route of administration can also affect the speed and duration of a drug's action, as well as its potential for side effects.
Local routes of drug administration
- Topical: external application of the drug to the surface for localized action, on skin or mucous membrane. In dental practice antiseptics, astringents, haemostatics are often applied as paints, toothpastes, mouthwashes, gargles or lozenges.
- Deeper tissues (but local effect): eg. infiltration around a nerve (Lidocaine).
- Ocular: This involves administering a drug directly to the eye, such as with eye drops or ointments for the treatment of eye infections or inflammation.
- Otic: This involves administering a drug directly to the ear, such as with ear drops for the treatment of ear infections or inflammation.
- Dermal: This involves administering a drug directly to the skin, such as with creams or gels for the treatment of skin conditions or for local anesthesia.
- Transdermal: This involves administering a drug through the skin, such as with a patch for the delivery of medications such as nicotine or hormones.
- Vaginal: This involves administering a drug directly to the vagina, such as with a cream or suppository for the treatment of vaginal infections or dryness.
- Rectal: This involves administering a drug directly to the rectum, such as with a suppository for the treatment of constipation or for local anesthesia.
Systemic routes of drug administration
- Enteral (GIT).
- Parenteral (other than GIT) (Injection).
- Others (Inhalation).
- Oral: This is the most common route of administration and involves taking a drug by mouth in the form of a pill, tablet, or liquid.
- Parenteral: This involves administering a drug through injection, either intravenously (into a vein), intramuscularly (into a muscle), or subcutaneously (under the skin).
- Inhalation: This involves breathing in a drug in the form of a gas or mist, such as with an inhaler for the treatment of respiratory conditions.
- Intranasal: This involves administering a drug through the nasal passages, such as with a nasal spray.
Factors governing choice of route
- The nature of the drug: Certain drugs are better suited for certain routes of administration. For example, some drugs are not well absorbed when taken orally and are therefore given by injection.
- The desired therapeutic effect: The desired therapeutic effect is a major factor in choosing the route of administration. For example, if a rapid and intense effect is desired, an intravenous (IV) injection may be the best option. On the other hand, if a slower, sustained effect is desired, an oral route may be more appropriate.
- Patient factors: The age, health status, and individual characteristics of the patient can impact the choice of route. For example, some routes may not be suitable for young children, elderly individuals, or patients with certain medical conditions.
- Ease of administration: The ease of administration is also a factor, as some routes may be more convenient or less invasive than others.
- Absorption: The rate and extent of drug absorption can be affected by the route of administration. For example, some drugs are rapidly absorbed through the mucous membranes of the mouth or nasal passages, while others may be poorly absorbed through these routes.
- Distribution: The distribution of a drug throughout the body can also be influenced by the route of administration. For example, some drugs are rapidly and widely distributed when given intravenously, while others may be poorly distributed through this route.
- Metabolism and elimination: The metabolism and elimination of a drug can be affected by the route of administration, as well as the patient's age, health status, and individual characteristics.
- Cost: The cost of a drug and the equipment required for administration can also impact the choice of route.
- Oral routes of drug administration
- Safe.
- Convenient.
- Economic.
- Variable absorption.
- Slow action.
- Unsuitable in consciousness.
- Unsuitable for acid unstable drugs.
- Food interaction.
- 1st-pass effect
Sublingual /Buccal routes of drug administration
- Avoid hepatic first pass - Bioavailability is higher.
- Rapid absorption – due to the good blood supply.
- suitable for small doses only.
Rectal routes of drug administration
- Useful in pt with a vomiting or unconscious.
- Rapid absorption than oral.
- Irregular or incomplete absorption .
- Mucosal irritation.
Inhalation routes of drug administration
- Suitable for local and systemic administration.
- Poor ability to regulate dose.
- Complex method of administration
Parenteral Routes routes of drug administration
- Rapid and immediate effect.
- Suitable in emergency.
- Suitable for large volume and for painful and irritating substance.
- Need trained person and a septic precaution.
- Difficult to recall drug after administration (unsafe).
2. Intramuscular (IM)
- Suitable for depot formulation (oily).
- Rapid absorption than oral.
- Need trained person.
- Pain and tissue damage during injection.
3.Subcutaneous :
- Suitable for slow released preparation.
- Not suitable for large volume.
4-Intradermal:
(into the skin itself) is used for skin testing some allergens.
5-Intrathecal:
6-Intraperitoneal:
Topical:
- Applied for local effect in the:
- Skin.
- Eye.
- Ear.
- …..etc







No comments